Pregnancy is a time of rapid change in all aspects. Hormones and mechanical factors work together to quickly demand something completely new of the body. It’s not unusual for these demands to cause aches and pains, but that doesn’t mean it’s something you necessarily have to tolerate.
Changes in Pregnancy
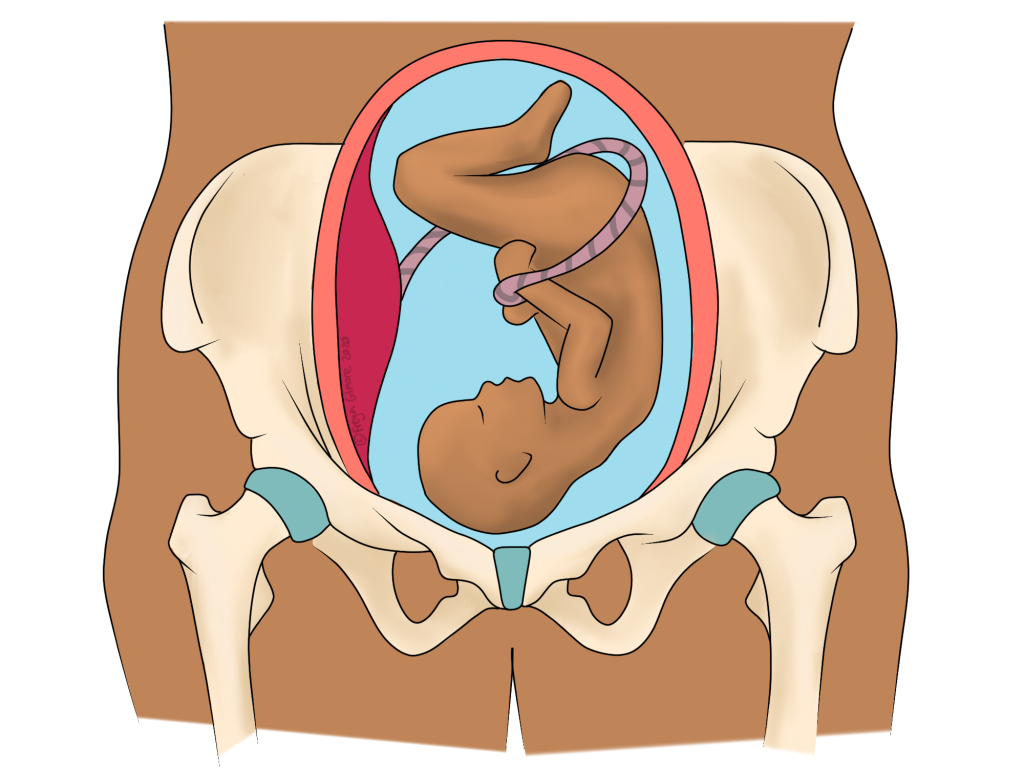
Whereas some patients expect pain in pregnancy, others are surprised or even worried to have it. The explanation of what’s going on makes them feel more at ease. During pregnancy, the body prepares the pelvis to move in new ways and allow the baby through the birth canal. This requires a lot of the aptly named hormone “relaxin”. This hormone increases the laxity of ligaments, especially around the pelvis. By allowing more movement through the pelvis, the muscles around it have to work harder to keep it stable. This, combined with a growing weight on the front of the abdomen, leads to achey buttocks and lower back muscles. Sometimes it can also lead to piriformis syndrome too.
Jarring movements like stepping off a kerb tend to bother the joint itself, which might feel like a deep ache. It’s not unusual for pain to flip from side to side, or even manifest in the front of the pelvis. The pelvis is like a ring when viewed from above, so it makes sense that if forces change through one part of it, that another part will adapt.
SPD and PGP: Lower Back and Pelvic Joint Pain
The abbreviations “SPD” and “PGP” are thrown around a lot in pregnancy. SPD refers to dysfunction of the pubic symphysis (Symphysis Pubis Dysfunction), which is the joint at the front of the pelvis. “Dysfunction” in this case is a broad term, and typically does not refer to any injury or damage. PGP stands for Pelvic Girdle Pain, which encompasses both SPD and pain over the sacroiliac joints (SIJs). Symptoms can occur within all three joints- if you imagine the pelvis as a ring or a bowl this makes sense. A problem in one joint will cause compensation through the other two.
The main reason these joints can be irritated during pregnancy is due to the hormone relaxin. As the name suggests, it causes structures to relax: specifically ligaments. The pelvis is very stable and usually the role of its joints are for shock absorption. But during vaginal delivery, the bones need to move to make room for the baby to exit. Evidence shows that birthing in positions that allow the sacrum (bone in the centre of the pelvis at the back) to move “might be favourable to facilitating spontaneous birth”. So movement is important, at least during birth.
However, just like you might have gone up a cup size or two well before the third trimester, relaxin can kick in early too. Relaxin is produced from the first trimester. It is estimated that SPD may feature in up to 1/4 of pregnancies.
Symptoms
Both SPD and PGP are often unnoticeable at rest. Pain over the front or back of the pelvis, or into the groin, tends to only peak on movement. Changing position, such as going from sitting to standing, is a common trigger. Turning in bed can also be painful. Weight bearing on one side, for example when leaning to one side to pick something off the floor, can be particularly uncomfortable.
Walking or other repetitive movements may initially be a trigger, but can often reduce the pain and be useful as a management strategy.
Management
Strengthening the muscles around the pelvis before and during pregnancy may be a way to minimise symptoms. Muscles in question include the lower back, buttocks, hamstrings, and quadriceps.
Identifying patterns is an important part of working out a strategy. You may find that the day after particularly strenuous activity symptoms are worse, but the next day you are pain free. Finding the sweet spot for a comfortable level of daily activity is possibly the easiest fix.
As with most things- the sooner you can make changes the better. Most* PGP resolves at birth, but suffering can typically be reduced beforehand. Don’t wait til you’re on crutches to see your osteopath! You may prefer to see an osteopath who specialises in treating pregnant women, although PGP is not too different to other types of back pain.
Alongside treatment for the joints and muscles that act on the pelvis, your osteopath can give you advice to keep the area happy up to birth. This may include specific exercises tailored to you, or more general advice on how much movement could be right for you. Ideas for adapting the way you sit, sleep, and move generally can also help. They may also recommend crutches or supports if they are things you would like to try.
Carpal Tunnel Syndrome
A nerve running down the arm and into the palm of the hand – the median nerve – is relatively vulnerable to compression at the wrist. When this happens, you may experience pain, numbness, weakness, or tingling in the hand. This is carpal tunnel syndrome, and although there are many possible causes, one common mechanism is repetitive movements involving a lot of wrist flexion: bending the wrist so the palm is closer to the forearm. This movement causes direct compression to the carpal tunnel itself, through which the nerve runs.
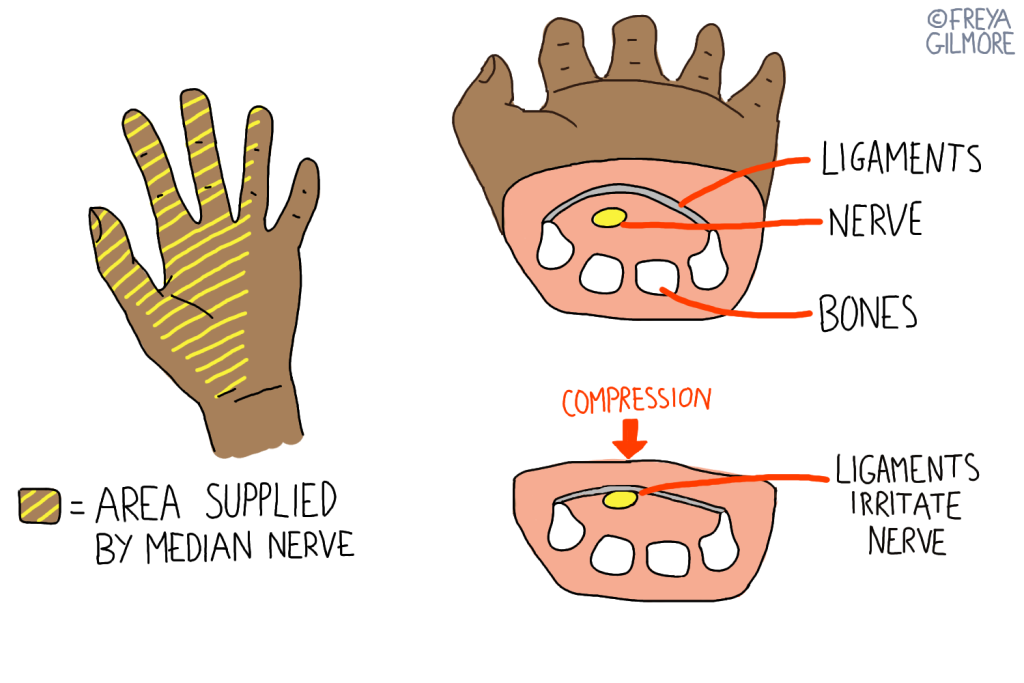
The carpal tunnel is found on the palmar side of the wrist and is made of the bones of the wrist deep in the hand and a set of ligaments close to the surface. As the wrist is flexed, the softer ligaments are compressed but the wrist bones stay put, meaning the tunnel and its contents are squashed. This can cause irritation to the median nerve over time. Nerves can continue to react once a stimulus is removed, so improvement may take time.
Other Potential Causes of Hand Pain
Pregnancy can increase the likelihood of a patient developing carpal tunnel syndrome as general fluid retention increases the pressure within the wrist, meaning less compression is required to affect the median nerve. Similarly, local swelling caused by trauma, or conditions like lymphoedema can add pressure to the carpal tunnel.
The symptoms can be confused with other conditions, for example Thoracic Outlet Syndrome, where a nerve is irritated on its route around the neck and shoulder. Your osteopath will be able to use hands-on testing to work out where the irritation is coming from, and therefore work out which area needs to be treated.
Osteopathic treatment may involve techniques to reduce swelling and demand, using a wrist splint overnight, or working out how to alter daily life to avoid excessive wrist flexion for a mechanical cause as described.
Pregnancy Related Cramping
Please note that this section refers only to muscular cramps- abdominal cramps should be discussed with your midwife.

Cramps are recognised as a symptom that your osteopath may be able to help with. There are times in a person’s life when cramps become more common, and pregnancy is one of these. Leg cramps tend to affect expectant mothers in the third trimester primarily, which may be down to a combination of things:
- increased water retention causing nerve irritation (as with carpal tunnel syndrome)
- increased demand on the muscles on the back of the body causing fatigue to the calf, hamstrings, glutes
It would make sense that an osteopath could help you to manage cramps associated with overworked muscles. Although we can’t change that your centre of gravity has moved, we can see if any other areas are underworking and adding to the strain. We can also give you stretches that might help either in the moment or for general management.
